Cancer cells are not alone: As cancerous tumors grow unregulated cancer cells engage other cells, in their path of destruction like macrophages which are part of the immune system and endothelial cells which make blood vessels. This collection of non-cancer cells that powers cancer growth is called the tumor microenvironment. How does the tumor microenvironment help cancer cells proliferate even more?
Answering this question is a holy grail of cancer science and holds the key to new therapies. Cancer cells, with their many mutations and unchecked DNA damage, change constantly: they can be a moving target for therapy and develop resistance to drugs that seemed to work at first. The non-cancer cells in the tumor microenvironment are genetically stable. If we knew how these cells interact we could to stop the tumor microenvironment from feeding the cancer, halt cancer growth or even reverse it. On February 28 a team of SKI scientists published a significant advance. The answer—surprisingly—is in metabolism.
All cells rely on metabolism, the engine-like process that requires constant fuel and oxygen to run. Cancer cells have altered metabolisms: they consume lots of oxygen and dump metabolic waste such as lactic acid. Because of this, cancerous tumors should only grow so large before the toxic effects accumulate like pollution in a jam-packed city, and eventually slow cancer growth. This is prevented, however, by tumor-associated macrophages (TAMs) that respond to the harsh environment and start a tissue-repair mechanism to clean it up.
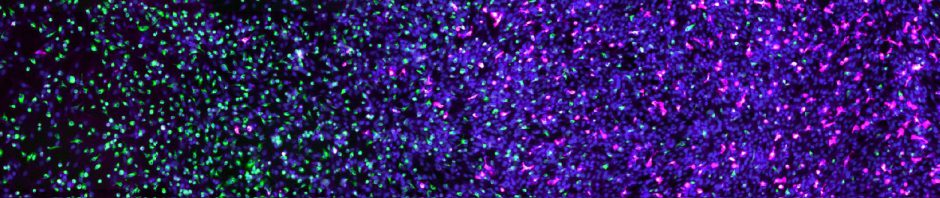
The SKI team started by observing the behaviors of TAMs in a mouse model of cancer. Then, they fabricated tissue-mimetic systems to recreate the same process in vitro. Using this approach they discovered that TAMs respond to low oxygen and to the presence of lactic acid and start producing a vascular endothelial growth factor (VEGF). This growth factor commands endothelial cells to start producing blood vessels—called neo-angiogenesis—a process that can bring new blood to struggling cancer cells, replenishing oxygen and removing toxic waste.
The tissue-repair response of macrophages is normally a good thing: it is how our body heals wounds and clears out toxic waste from muscles after intense exercise. In cancers, however, it can make cells with complementary skills—cancer cells, TAMs and endothelial cells—work together in a terrible way. Rescuing cancer cells from dying because of their own altered metabolism boosts the cancer to grow even more.
The SKI study established a new role for cancer metabolism in the interactions between cancer cells and their microenvironment. These findings lay the foundations for our understanding of cancer development, diagnosis and treatment.
But the study also showed how an interacting team of multidisciplinary scientists could answer a difficult cancer question: Craig Thompson brought his expertise in cancer metabolism, Johanna Joyce her expertise in the tumor microenvironment, and João Xavier his expertise in cancer systems biology, a new field that aims to integrate cancer concepts. Cancers subvert cells with complementary features in their path to destruction; figuring out its complex mechanisms—and new ways to fight them—may require teams of scientist with complementary skills.
The study was spearheaded by Carlos Carmona Fontaine, former postdoctoral researcher at MSKCC who is now assistant professor of Biology at the New York University.
Metabolic origins of spatial organization in the tumor microenvironment
Carlos Carmona-Fontaine, Maxime Deforet, Leila Akkari, Craig B. Thompson, Johanna A. Joyce, Joao B. Xavier. PNAS
[Open Access]